Multiple Sclerosis: A Deep Dive into History and Causes
Tanush Gupta
Introduction
Multiple sclerosis (MS) is a chronic (long-term) autoimmune disease that affects the central nervous system (CNS), causing damage to the protective myelin sheath around nerve fibres. This disruption interferes with the transmission of nerve signals, leading to a range of neurological symptoms. With approximately 2.9 million people worldwide (1) living with MS and nearly 7,100 people getting newly diagnosed with MS each year in the UK (2) , the urgency to advance research, improve diagnostic tools, and develop more effective treatments has never been greater. MS is most commonly diagnosed in young adults, with women being two to three times more affected than men (1) . This article will explore the history of MS, its causes, and symptoms, laying the groundwork for our next article on diagnosis and treatment options.
Historical Background
MS has likely existed for centuries, but the first documented case is often linked to Saint Lidwina of Schiedam in the 14th century (3), who experienced progressive neurological problems. However, it wasn't until 1868 that French neurologist Jean-Martin Charcot (pictured right) provided a clear description of the disease. He called it "sclérose en plaques" because of the hardened patches, or plaques, found in the brain and spinal cord of MS patients(4). Charcot also identified a trio of common symptoms (known as "Charcot’s triad."): nystagmus, tremors and dysarthria.
Importance of Myelin:
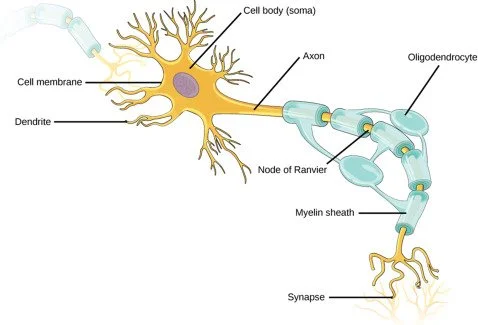
MS is caused by a mix of genetic and environmental factors that lead to an immune system malfunction. Instead of protecting the body, the immune system mistakenly attacks the myelin sheath, leading to nerve damage and impaired communication between the brain and
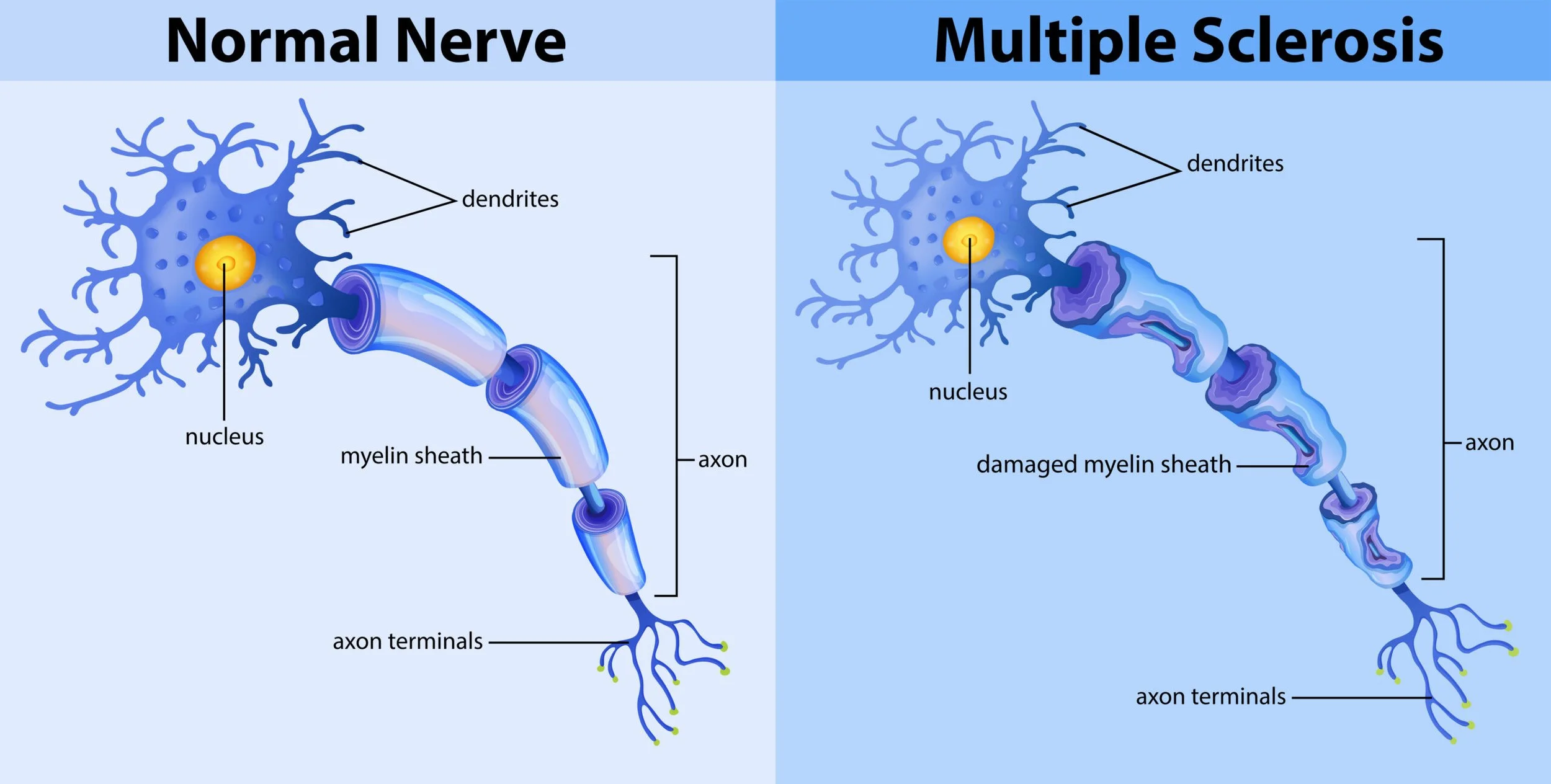
body. Myelin acts as an insulating layer around nerve fibres, like the coating around electrical wires. This insulation allows nerve impulses (electrical signals) to travel quickly and efficiently along the axon (the long, thread-like part of a neuron). When the myelin sheath is damaged, as in MS, several problems arise. Myelin speeds up nerve conduction by allowing signals to "jump" between gaps called Nodes of Ranvier. Without myelin, the signal moves more slowly or may not reach its destination . Damage to myelin can also cause nerve impulses to become weak or stop entirely before reaching their target muscles or other neurons resulting in signal disruption (conduction block) . This can lead to symptoms like muscle weakness, vision problems, or numbness . In some cases, demyelination causes "cross-talk" between nerve fibres, where signals spread incorrectly to neighbouring neurons resulting in erratic or misdirected signals. This can result in symptoms like involuntary muscle contractions, tremors, or sensations like tingling or electric shocks.
How the Immune System Attacks Myelin & Risk Factors
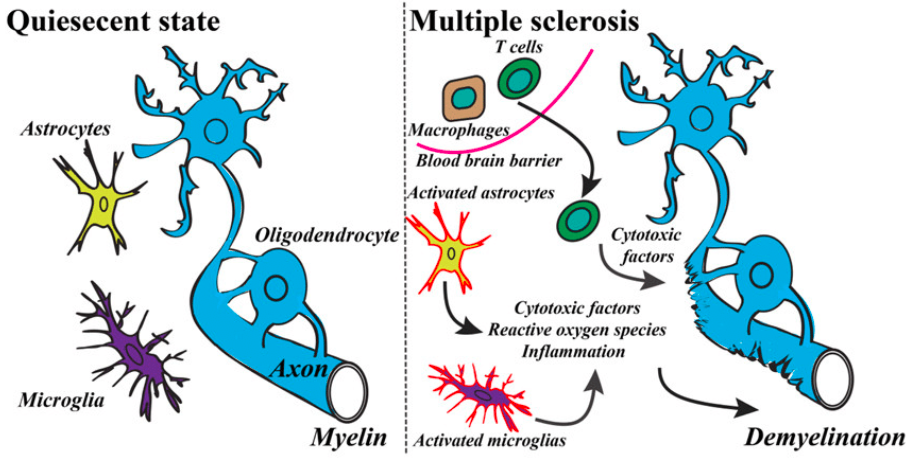
A key component of MS is the abnormal activity of immune cells, particularly T Helper cells and B cells: T cells mistakenly recognize myelin as a foreign invader and trigger inflammation, which damages nerve fibers. B cells, which usually produce antibodies to fight infections, also play a role in attacking myelin. This immune attack leads to scarring (sclerosis) of myelin sheath and the breakdown of nerve function over time.
Scientists haven't identified exactly why some people develop MS, but research suggests a combination of: Genetic Predisposition and Environmental triggers.
Certain genes, especially those in the HLA-DRB1 region, increase the likelihood of MS by influencing how the immune system differentiates between self and non-self proteins. Variants of HLA-DRB1 (5) can cause immune cells to mistakenly recognize components of myelin as foreign, leading to an inappropriate immune response and chronic inflammation.
It has also been observed that high salt induces inflammation in a type of immune cell known as CD4 T cells, while also causing a loss of regulatory T cell function. This, they found, is mediated by a salt-sensitive kinase, or enzyme critical for cell signaling, known as SGK-1. For a study, researchers used RNA sequencing to compare gene expression in patients with MS with expression in healthy individuals. In patients with MS, the researchers identified upregulation, or increased expression, of a gene called PRDM1-S (primate-specific transcription factor), also known as BLIMP-1, which is involved in regulating immune function. Surprisingly, PRDM1-S induced increased expression of the salt-sensitive SGK-1 enzyme, leading to disruption of regulatory T cells, the researchers found. Moreover, they found similar overexpression of PRDM1-S in other autoimmune diseases, suggesting that it may be a common feature of regulatory T cell dysfunction (6).
Vitamin D also plays a crucial role in immune regulation (6) by helping to keep immune responses balanced. It enhances the function of regulatory T cells (Tregs), which suppress excessive immune activity and prevent the immune system from attacking the body's own tissues. Low vitamin D levels can weaken this regulation, allowing an overactive immune response that mistakenly targets myelin, increasing the risk of MS.
Epstein-Barr virus (EBV) , the virus responsible for infectious mononucleosis (commonly known as "mono" or the "kissing disease" due to spread by saliva and common in teenagers), has been strongly linked to MS (7). EBV causes mononucleosis by infecting B cells and triggering an immune response. This leads to the production of atypical lymphocytes, which are a hallmark (characteristic sign) of the disease and cause symptoms like swollen lymph nodes,spleen, liver , sore throat and liver. After infection, EBV remains dormant in the body but can alter immune function. One proposed mechanism is molecular mimicry, where EBV proteins share structural similarities with myelin proteins. As a result, the immune system, once primed to attack EBV, may mistakenly target myelin, triggering an autoimmune response. A second important finding was that these cross-reactive T-cells can be found in people with MS but also in those without the disease. This suggests that differences in how these immune cells function may explain why some people get MS after EBV infection.
Another environmental risk factor is cigarette smoking (8). Cigarette smoke contains harmful chemicals that promote oxidative stress, a state where reactive oxygen species (ROS) accumulate in cells faster than they can be neutralized by antioxidants. This imbalance damages cells, including neurons and myelin-producing oligodendrocytes (type of glial cell - non neuronal cells which support and maintain neuronal cells) reducing myelin repair and increasing risk of demyelination (9)(10). Oxidative stress promotes inflammation by activating immune cells, such as microglia and astrocytes. They release inflammatory cytokines like TNF-α and IL-6.
This inflammation makes it more likely that T cells and B cells will attack myelin. Furthermore , when myelin is damaged by oxidative stress, the breakdown products can be picked up by antigen-presenting cells (like dendritic cells), which may mistakenly present them to T cells as foreign, triggering an autoimmune response. Oxidative stress weakens the blood-brain barrier, making it easier for immune cells that normally wouldn't enter the central nervous system (CNS) to invade and attack myelin. Chronic oxidative stress disrupts immune regulation, making it more likely that the immune system will attack myelin, thus worsening MS progression.
Furthermore , growing up in regions farther from the equator like New Zealand, Canada, and Scotland (1) is associated with a higher risk of MS. This is likely due to lower sunlight exposure, which results in lower vitamin D production. Additionally, childhood exposure to infections varies by geography. In tropical regions, frequent exposure to various pathogens may help train the immune system to develop tolerance, reducing the likelihood of autoimmune diseases. In contrast, temperate regions may have different infection patterns that do not provide the same immune regulation, potentially leading to an increased risk of MS.
Symptoms
in multiple sclerosis (MS), re-myelination does occur, but it often cannot keep up with the rate of demyelination. Early in the disease, oligodendrocytes (the cells responsible for producing myelin) attempt to repair the damage, leading to some degree of re-myelination. However, over time, this process becomes less effective due to chronic Inflammation (persistent immune attacks damage oligodendrocytes and impair their ability to regenerate myelin) , oligodendrocyte loss (with repeated demyelination, fewer oligodendrocytes remain to restore myelin) , gliosis (scar formation - astrocytes form scars (sclerosis) that physically hinder re-myelination) and age and disease progression (As MS advances, the body's ability to remyelinate declines).
The scarring (sclerosis) occurs in the myelin sheath , when T cells and B cells mistakenly attack myelin, causing inflammation and damage, leading to the formation of lesions or plaques. These plaques are essentially areas where the myelin has been stripped away, and as the disease progresses, these lesions can develop into hardened scar tissue - sclerosis." This scarring disrupts the normal conduction of electrical impulses along the nerve fibres, leading to the neurological symptoms of MS such as muscle weakness, coordination problems, and cognitive impairment (11).
MS symptoms vary widely, depending on which part of the CNS is affected. Some common early signs include vision problems (optic neuritis due to inflammation
of optic nerve), muscle weakness, numbness, and difficulty with balance and coordination (all due to disruptions in normal transmission of nerve signals) (12).
Conclusion
Multiple sclerosis is a complex disease with a fascinating history and a challenging diagnostic process. While we now understand much about its causes and progression, there is still no cure. However, significant progress has been made in treatment, which will be the focus of our next article, where we explore the diagnosis, latest therapies and future research directions.
References:
(1) https://www.mssociety.org.uk/what-we-do/our-work/our-evidence/ms-in-the-uk
(2) The number of people living with MS in the UK increases | MS Trust
(3) https://multiplesclerosis.net/living-with-ms/history
(4) https://mymsaa.org/ms-information/overview/history/
(5) https://pubmed.ncbi.nlm.nih.gov/9777330/
(6) https://www.sciencedaily.com/releases/2024/08/240828224252.htm
(7) https://www.sciencedaily.com/releases/2024/06/240606152402.htm
(8) https://www.jocn-journal.com/article/S0967-5868(14)00168-4/abstract
(9) https://pubmed.ncbi.nlm.nih.gov/8102159/
(10) https://pubmed.ncbi.nlm.nih.gov/7777166/
(11) https://pmc.ncbi.nlm.nih.gov/articles/PMC5241505/#B58
(12) https://pubmed.ncbi.nlm.nih.gov/24507522/
Key Terms & Definitions:
Autoimmune disease: body’s immune system mistakenly attacks its own healthy cells
Nystagmus: Involuntary eye movements that can affect vision.
Dysarthria: Difficulties with speech, which can manifest as slurred or slow speech
T helper cell: is a type of white blood cell within the immune system that plays a crucial role in coordinating the body's response to infection by activating other immune cells, like B cells and cytotoxic T cells, to effectively fight off pathogens; essentially, they "help" other immune cells do their job, hence the name "helper" cell. Also known as CD4+ T cells because they express the CD4 protein on their surface.
B cell: A type of white blood cell that makes antibodies
Microglia and Astrocytes : Glial cells in the CNS that support neurons and maintain homeostasis and are both part of the innate immune system and play a role in neuroinflammation
Cytokines: small proteins that are crucial in controlling the growth and activity of other immune system cells and blood cells
Blood Brain Barrier: The blood-brain barrier (BBB) is a semi-permeable membrane that protects the brain from harmful substances and regulates the movement of nutrients and other molecules in and out of the brain
Lesion : any abnormal tissue change or injury. It can be caused by disease, trauma, or other factors. - Lesions in MS are areas of damaged myelin, the protective sheath around nerve fibres in the central nervous system
Plaques are a specific type of lesion that is characterized by a distinct, hardened area of damaged tissue. Plaques refer to the hardened, scar-like areas that form when myelin is damaged and replaced with scar tissue (sclerosis). These plaques are seen on MRI scans as bright spots in the brain or spinal cord and indicate areas where the myelin has been stripped away and replaced by scar tissue
Synoptic Links to AQA A level Biology
Topic 3.2.4 - Cell recognition and the immune system
Topic 3.6.2 - Nervous coordination
Topic 3.8.4 - Gene technologies allow the study and alteration of gene function allowing a better understanding of organism function and the design of new industrial and medical processes